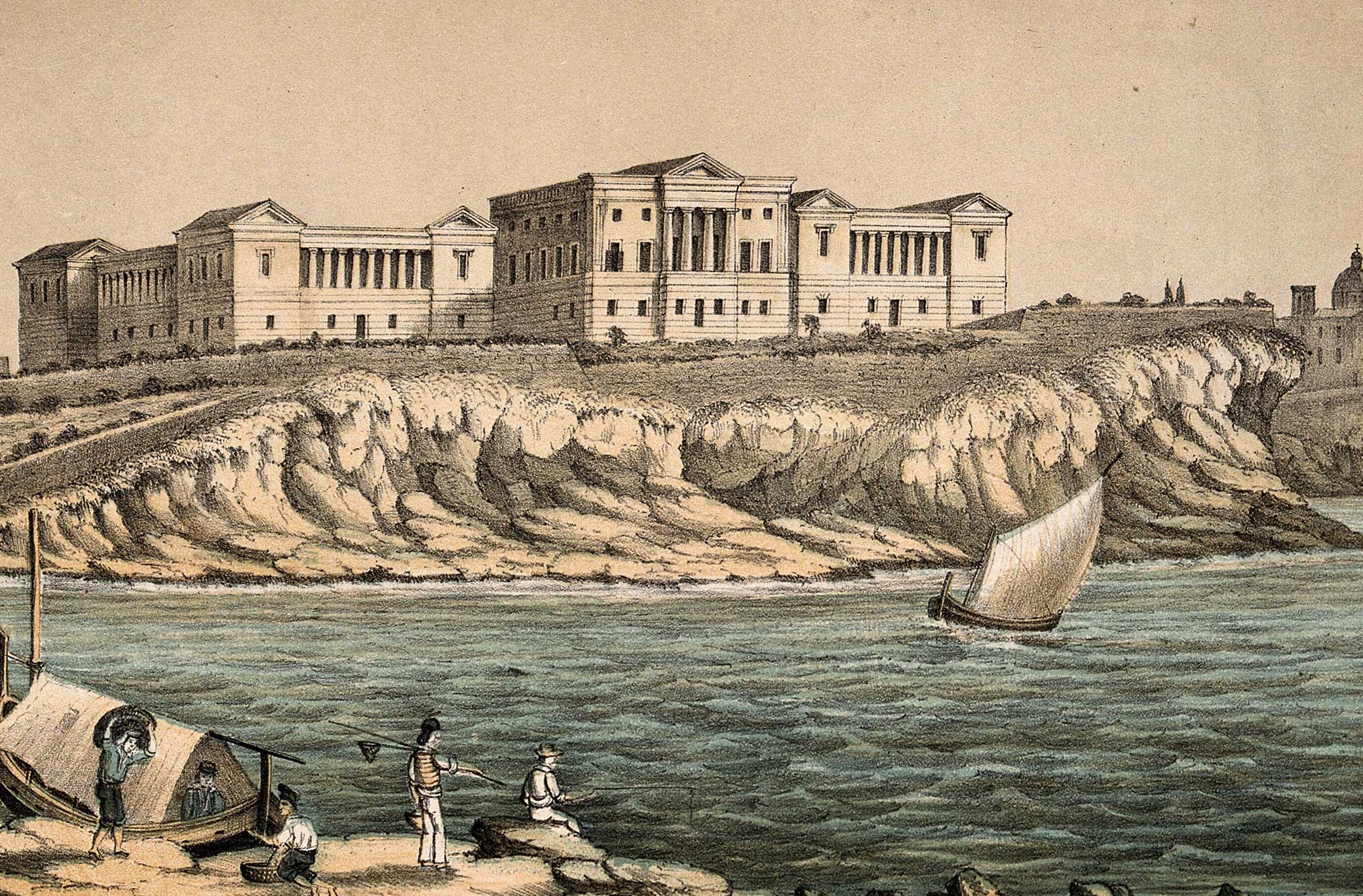
Royal Naval Hospital in Malta. Wellcome Collection.
We don’t know the name of the laundress who washed the dirty linen of travelers quarantined on the Mediterranean island of Malta in the 1830s—travelers who had arrived by ship from plague-ridden cities like Alexandria. We do know that she lived in Valletta, the capital of British-controlled Malta, probably near the gardens that overlooked the harbor. Passengers on ships from North Africa and the Middle East that stopped in Malta, a hub for maritime traffic in the Mediterranean, were required to undergo quarantine before continuing on to Europe.
Those on ships that either had known cases of disease or were suspected to be carriers were given a “foul bill of health” and quarantined for a longer period. While some crew members remained on the ship, most passengers disembarked and were lodged in the lazaretto, a large stone hospital and quarantine facility on a small island in the main harbor of Malta. Soiled linen from the ship would be collected and delivered to the laundress, who was quarantined along with the passengers in the lazaretto. Working in the dank basement, she would likely have hauled buckets of water and armfuls of wood to boil clothing in large vats. She would soak the clothes overnight to begin the process of removing the stains and smell. The next morning, she would begin the arduous process of scrubbing the fabric. She would use alcohol to remove bloodstains, chalk and pipe clay to remove grease stains, and even urine as bleach, grinding these potpourri ingredients into the clothing. The clothing would then be hung outside to dry in the Mediterranean sun.
Laundresses in Malta followed this routine of cleaning soiled linen for decades. The clerk of the lazaretto in the 1830s, Giovanni Garcin, noted their routines, their labor, and their health. Despite being in direct contact with the dirty linen, he testified, none of the laundresses he had observed in his twenty-nine years of employment had become infected with plague. This testimony appeared in a treatise by the British physician Arthur T. Holroyd that presented an argument against the practice of quarantine. The fact that plague did not spread from soiled linen to laundresses was one piece of evidence Holroyd brought forward to prove that plague was not contagious.
The treatise was addressed to Sir John Cam Hobhouse, a British member of Parliament who spearheaded various reform efforts and was president of the Board of Control for India. Holroyd contended that existing quarantine regulations were unnecessary, expensive, and outdated. The laundresses likely had no idea that they served as an example to help understand how disease spread (or didn’t spread). Who the laundresses were, what they thought as they entered quarantine, and whether they feared working with linens from infected ships did not matter to those who observed them. The reference to the laundresses in Holroyd’s treatise appears on just two pages, but it was an important clue in undermining the prevailing belief that plague was contagious.
Such bits of evidence were not uncommon throughout the late eighteenth- and early nineteenth-century quarantine debates. They appear as short statements, sparsely worded phrases, parenthetical notes, and elliptical references in reports by doctors and quarantine officials about infectious diseases. These people helped the medical community and government agencies visualize how disease spread.
During the early nineteenth century, many British physicians began to doubt the theory that underlay quarantine regulations. Plague, cholera, and certain other epidemic diseases had for long been thought to spread through contagion—direct contact with a sick person or with objects the person had come into contact with. Battle lines were drawn up between contagionists and anticontagionists, the latter supported by merchants who wished to do away with the costly quarantine system. To disprove the contagion theory, physicians often turned to hospital workers, who had close proximity to the sick. The hospital workers’ health became a barometer to determine the contagiousness of disease.
For his book on plague and quarantine, Holroyd created a questionnaire for doctors and administrators who worked in British hospitals and quarantine centers in Egypt and Malta. Questions concerned everything from sanitary conditions to incubation time and contagion. Holroyd posed questions to Thomas Leslie Gregson, chief surgeon of the naval hospital in Alexandria. When asked if he had observed “disease propagated by contagion,” Gregson stated that he had not seen any cases and that in fact “on investigation have found many so reported to be false.” Gregson’s use of the term investigation is an indication of the shift to a more scientific approach to medicine that was taking place in the nineteenth century.
The questionnaire’s format enabled Gregson and the other doctors to document their insights, observations, and analyses. In these narrative spaces, doctors followed well-established patterns of using dispossessed people to track the spread of epidemics. In the case Gregson reported about the “black” servant at his hospital who came down with plague, he argued that the infection resulted not from contagion but from the servant’s living conditions. Three other servants became infected at the same time, and “these four had their huts together.” Gregson’s comment that anyone who has seen an Arab hut “could easily conceive this happening” illustrates how familiar images of the Middle East were among physicians, and how such places could be easily conjured in their collective imagination. Commenting on Gregson’s observation, Holroyd concluded, “Egypt is never entirely free from plague, partly from atmospheric causes, and partly from local circumstances dependent upon the physical condition of the people…but mainly to the small, close, confined, and huddled huts which compose an Arab village, and which are always the hotbeds of the malady whether sporadic or epidemic.” Colonialism in Egypt allowed Gregson and other European physicians to witness and describe the conditions that they believed fostered the spread of plague.
As part of his concluding remarks in the book, Holroyd faulted the Board of Health of Alexandria for inefficiency, “inasmuch as it has never collected evidence respecting the plague, to show how the disease might be diminished or eradicated by improving local circumstances and the physical conditions of the people.” It is notable that Holroyd did not fall back on a racial argument that blamed the spread of disease on the Arab population but instead blamed it on those with power. He also did not put forth a climatic argument. Instead, he pinpointed the failures of the city policy and the poor structure of housing as the cause. The poor people’s living conditions in the Arab huts helped to make this claim visible.
Holroyd and others argued against contagion theory by contending that plague resulted from unsanitary conditions and crowded spaces. Being abroad encouraged some physicians to question medical dogma. Because of colonialism, doctors like Gregson had more ability to investigate the link between social conditions and health. Holroyd’s treatise on quarantine built on a growing body of medical literature by doctors who were stationed in India and other parts of the British Empire and were focused on the physical and social environment, including the climate and conditions of dirt and overcrowding, as the cause of illness.
By focusing his investigation on what doctors and administrators in colonial settings had discovered about the health of communities, rather than individuals, Holroyd was operating like a public health investigator. Holroyd’s major objective was to present a convincing argument against quarantine restrictions, which a growing number of physicians had begun to view as ineffective, by showing that plague was not contagious.

To further illustrate this claim, he turned to Muslim pilgrims returning from the hajj, the annual pilgrimage to Mecca. Pilgrims returning from Mecca on ships to various Mediterranean ports were quarantined for up to several weeks in the lazaretto in Malta. Holroyd quoted Captain Bonavia, superintendent of the lazaretto, who described what happened on one ship full of pilgrims that stopped in Malta in February 1837. The ship arrived from Tripoli, Lebanon, with twenty-one Muslim passengers and a crew of eleven men. Because Tripoli was experiencing a plague outbreak, the ship was kept isolated in the harbor. Two pilgrims became ill with plague after arriving in Malta. One died on the ship, and the other was escorted to the lazaretto with two healthy companions; he died soon thereafter. The rest of the pilgrims were then disembarked and kept in quarantine for forty-one days, while the crew remained on the ship. One crew member died of plague ten days after the pilgrims had disembarked; the remaining crew were then taken off the ship and quarantined for another two weeks. None of the remaining pilgrims and crew became ill.
Holroyd concluded from this report that the plague could not be contagious, as it was not communicated from the plague victims to the others, despite their close quarters. The crew member could not have contracted the disease from the two stricken pilgrims, since he did not become sick until ten days after having been in contact with them. A more reasonable conclusion for why the crew member became infected, wrote Holroyd, was that “the vessel had not been properly ventilated” and “an impure atmosphere still existed.” The ship was sunk and then raised up again; when the crew returned, they remained healthy. “Surely it was the removal from the contaminated air and the purification of the vessel which prevented the extension of the pestilence.” Holroyd argued that both people and objects contaminated with plague could be “purified” if exposed to fresh air. In response to his questions, Captain Bonavia stated that no guardians who handled baggage or merchandise had ever come down with the plague. This included people who handled cotton, but any cotton articles coming from ships that had plague on board were “exposed to the air and ventilation before they are handled.”
Holroyd also reported data, obtained from Captain Bonavia, on the number of “passengers, troops, and pilgrims” who were quarantined in Malta. Between 1832 and 1837, Bonavia reported, roughly ten thousand passengers, three thousand troops, and two thousand pilgrims had been housed in the lazaretto. For the period from 1810 to 1832, the lazaretto clerk, Giovanni Garcin, reported that an average of eight hundred to a thousand people were quarantined annually. No one in the lazaretto, reported Bonavia and Garcin, had ever contracted the plague while in quarantine (unless coming from an infected ship). The lazaretto officials’ documentation of the number of people who were placed in the quarantine facility in Malta is an example of the kind of record keeping that became an important element of epidemiology. The simple task of record keeping, tallying the number of people in the facility, provided empirical evidence about how plague spread.
With the benefit of hindsight, it is possible to say that Holroyd was both right and wrong in his belief that plague is not contagious. While fleas, not humans, are primarily responsible for transmitting plague, it can be transmitted from person to person through the air in its pneumonic form. Holroyd’s contribution lies less in the accuracy of his argument about transmission than in the methods he used. Holroyd condemned Egyptian officials for not collecting evidence about plague. He believed that if physicians had recorded their observations, municipal officials would be better equipped to respond to the epidemic: “Surely medical men, who have seen much of the plague, ought to have been summoned to give all the information they possessed about the malady, with a view, if possible, to lessen the present oppressive and tyrannical laws.” In response to Holroyd’s questionnaire, Robert Thurburn, British consul in Alexandria, had stated that “the collection of evidence respecting the plague has never, so far as I know, been one of the objects of the Board of Health.” Similarly, Captain Bonavia reported that the Board of Health in Malta did not collect evidence from “medical men” about incubation period and other facts about the plague. The board, he stated, “acts according to the general regulations established and observed here from old date, without references to other medical evidence, excepting that of the local physicians when occasion requires it.”
The value of Holroyd’s report lies in helping to illuminate an overlooked aspect in the history of the British Empire’s approach to the study of infectious disease. Deployed across the empire, British physicians were assigned to provide medical care to troops and others in the colonies, and as they responded to medical crises in unfamiliar environments, they became investigators. The debates surrounding quarantine laws in the British metropole and elsewhere during this period provided further incentive to document health conditions, collect evidence, and write reports. In the process of writing these reports, British physicians often observed the spread of disease in populations throughout the empire. Their efforts, in turn, contributed to the development of methods that would come to be standard in modern epidemiology.
Adapted from Maladies of Empire: How Colonialism, Slavery, and War Transformed Medicine by Jim Downs, published by The Belknap Press of Harvard University Press. Copyright © 2021 by the President and Fellows of Harvard College. Used by permission. All rights reserved.
